
The future of healthcare architecture will be focused on efficiency, safety, flexibility, team input and putting the patient first. Lean Six Sigma provides ongoing process improvement toward these goals.
Rod Collman, AIA, sdg Architecture

My mother spent her last five years in a 15-bed assisted living facility that had a family-like and home-like atmosphere. The care was very personal, very hands-on by qualified staff and in an intimate setting that was very comforting for her. She had the same caregivers for the entire 5 years. As an Architect, I was impressed by this model of care.
During my career span of over 50 years, I have had the opportunity to be involved in many elder care and hospital facilities. It has always been difficult to depart from the stigma of a double-loaded corridor that most skilled nursing units feature, including most hospitals. A design for fifteen or fewer beds in a single building unit, each with their own caregivers and patients in a communal campus setting, (like my mother’s facility), allows for more highly trained, engaged and satisfied caregivers, happier patients, and less employee turnover. In an upcoming post, we will further explore the role of architecture in the changing world of healthcare design. Before we do, let’s look at current trends in healthcare and the challenges that will define its future architecture.
The future design of healthcare is more complex than ever before. A 2011 article in Health Facilities Management (HFM) magazine, “The Future is now: How 10 Forces are Changing Health Care Design,” addressed the changing structure of the medical care model, staffing shortages, falling reimbursements, focus on transparency and quality, and more. Of key importance is “…trying to make efficient design a substitute for a new model of care… a business model that moves the priority away from the relentless pursuit of more patients and more procedures and toward a greater emphasis on quality of care and better health at a lower cost.” How can we design future healthcare facilities to better provide operational efficiency, including keeping professional staff?
LEAN Six Sigma (LSS) is a process improvement methodology that is growing in use across industries, including healthcare architecture, designed to eliminate waste, maximize efficiency, drive profitability, and improve quality of service and outcomes – with continuing process improvement. It is an important approach for the design of efficient healthcare operations and architecture.
“The primary focus of LEAN is eliminating waste,” said Ellen Hargett, Director of Quality and Patient Safety at Emory Health Care, Retired. “The focus is not just on waste of staff resources and talent. Every healthcare facility has built-in waiting areas. You wait there until called, resulting in a waste of your time, a practice that does not put the needs of the customer first. Imagine a process so efficient there is no waiting room…”
Non Value Added Waste in Healthcare
-
Overproduction
-
Excess Inventory
-
Waiting
-
Unnecessary Movement of Patients
-
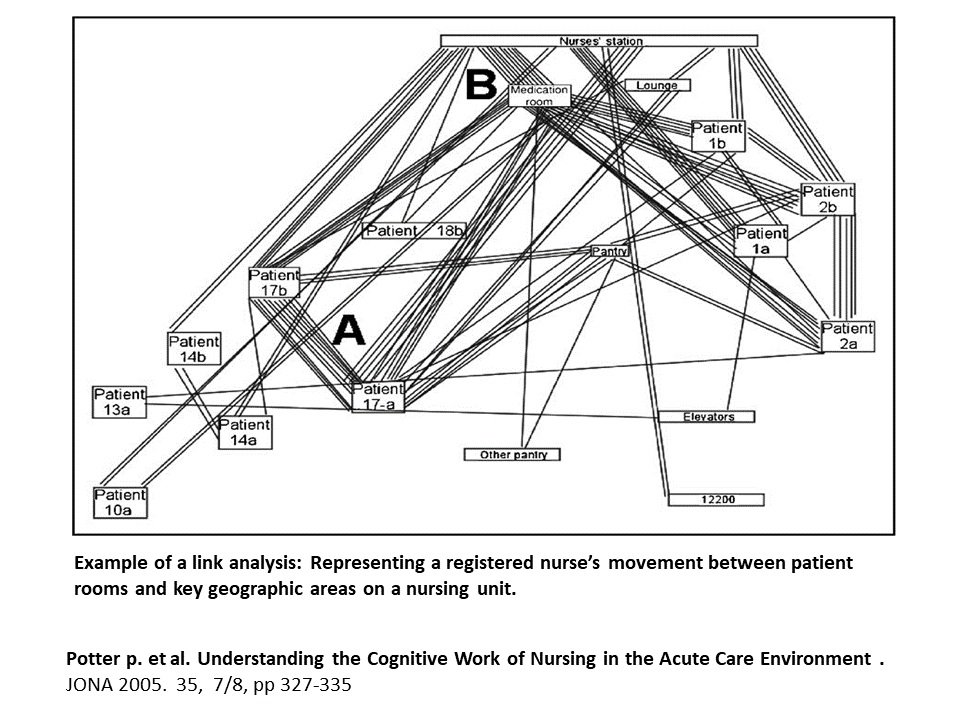
Unnecessary Movement of Employees
-
Unnecessary or Incorrect Processing
-
Defects Leading to Rework or Repair
-
Waste of Talent and Ideas
Arthur, J. Lean Six Sigma for Hospitals
She explains that CMS (Centers for Medicare & Medicaid Services) requires hospitals to report information on clinical outcomes (mortality, complication and readmission rates,) and service-related outcomes (satisfaction data from surveys of their consumers). Greater efficiency and less time spent through better utilization of staff create a more patient-centric process. Transparency regarding outcome impacts reimbursements as well as consumer loyalty.
“Through the collection and analysis of data such as patient-to-nurse ratios, room occupancy, patient waiting time, patient discharges for each day of the week, length of stay, unnecessary steps, and maximum use of staff, space and equipment; comparative throughput (the rate of operational production) can be improved,” said Hargett. “This is continuous process improvement.”
Healthcare providers must consider the needs not only of their consumers but also their employees. Hargett says the healthcare field (specifically nursing) is comprised of aging staff. A 2018 report from the American Association of Colleges of Nursing stated that the average age of a registered nurse (RN) in the U.S. is 50 years of age and that “Insufficient staffing is raising the stress level of nurses, impacting job satisfaction, and driving many nurses to leave the profession.”
Hargett reminds us that virtually all careers have opened to women. Statistics from www.census.gov indicate that men occupy only 9.6 percent of the U.S. nursing force. A two-year Associates Degree in nursing has historically landed a respectable job, but the profession’s demand is greater for a four-year Baccalaureate Degree and the rank of Registered Nurse (RN) than ever before. Working at the bedside is emotionally and physically demanding. It is hard for an aging workforce to function effectively in an often-inefficient architectural environment, additionally lacking the sensory aesthetics so important to the mental and emotional state of staff and patients. Hargett points out that traditional facility layouts and mandatory 12-hour shifts must be challenged if providers expect to retain valuable, experienced workers.
I recall that the assisted living facility where my mother lived showed signs that the LEAN process might have played a role in the design of the facility and how it operates. In an upcoming post, we will explore how LEAN, innovative technology and more comfortable environments can make future healthcare architecture more efficient, leading to less employee turnover; more highly trained, engaged and satisfied nurses and caregivers; and happier, healthier consumers.
Be the first to comment